![Tom Clark, far left, and Carl Eissman, in black apron on right, prepare food in Carley’s Carb-less Kitchen during a recent class for families learning to use dietary therapy to treat epilepsy.]()
When Carley Eissman started dietary therapy to manage epileptic seizures, her goal was simple — play basketball. She did not know that it would change her life or the lives of the many people who now receive dietary support and education in Carley’s memory.
After Carley’s 2011 death at age 19 in an accident related to an epileptic seizure, her family founded the Carley Eissman Foundation to benefit families who were beginning to use dietary therapy to treat epilepsy.
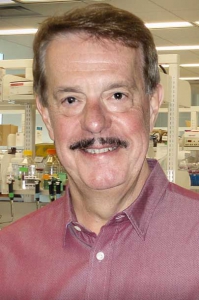
![Carley Eissman]()
Carley Eissman
As a teacher, Carley’s mother was not satisfied with simply raising and donating funds. “A good teacher gets on the carpet with the kids,” Lori Eissman said. “So I took that approach to my idea for a kitchen.”
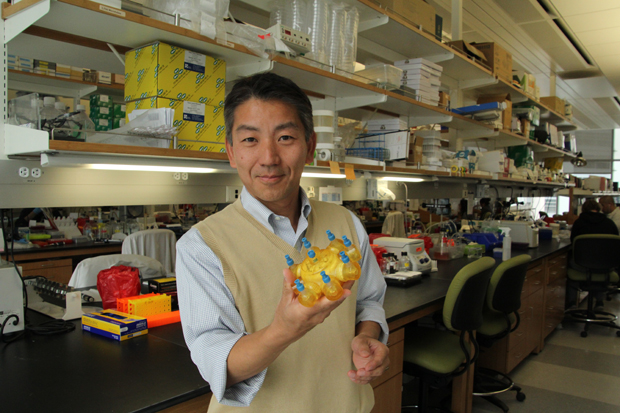
Today, Lori and Carl Eissman and other family members can be found cooking for a growing audience of families affected by epilepsy in Carley’s Carb-less Kitchen, which offers monthly cooking classes in cooperation with the dietary clinic at LAC+USC Medical Center.
“One of the things we keep talking about is that food really cuts across cultures and languages, and it is a really nice vehicle for effective human communication,” said Arthur Partikian, MD, director of child neurology at LAC+USC Medical Center and a specialist in epilepsy. “So it was a really unique idea to have a kitchen cooking class to introduce the concept of food as medicine.”
Epilepsy is a neurological condition that affects the nervous system and causes recurring seizures over time. More than 2 million Americans have epilepsy, according to the U.S. Centers for Disease Control. It is estimated that one in 26 people will develop epilepsy at some point in their lives.
Despite epilepsy’s widespread impact, the Eissmans and others have noted that it receives little attention outside of hospitals and academic research centers.
“Epilepsy has a very negative stigma about it because you don’t see it … until you have a seizure, and then it’s gone again.” Lori Eissman said. “There are so many people who never saw that Carley had seizures. They never understood it.”
The Eissmans are doing what they can to end the stigma. “People need to talk about epilepsy like they talk about cancer or diabetes,” Lori Eissman said.
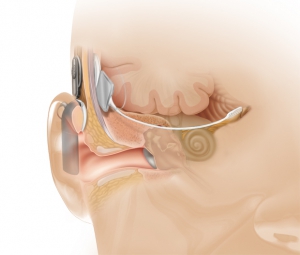
Treatments for the illness range from oral medication to brain stimulation and surgery. These treatments are often successful in controlling or even curing epilepsy, but one third of epilepsy patients live with uncontrollable seizures because no treatments work for them.
Carley Eissman was such a patient.
Laura Kalayjian, MD, chief of neurology and director of the EEG Lab at LAC+USC Medical Center, was the last of many physicians who treated Carley — but the first to suggest dietary therapy. Within a few months of strict adherence to a modified Atkins diet (MAD), Carley’s seizures had almost disappeared.
“These patients — many of them are determining whether or not to do brain surgery,” said Kalayjian, who is also an assistant professor of neurology at Keck School of Medicine of USC. “Sometimes dietary therapy is looked at as a last resort, and it shouldn’t be.”
Potential benefits to managing epilepsy through diet include weight loss and fewer negative side effects than surgery. But distinct challenges exist.
“Epilepsy is a socially isolating condition. Patients don’t have a lot of people to talk to,” said Jessica Lowe, a dietitian in the Department of Neurology who runs the dietary therapy classes. “When you put someone on this therapy, it changes their entire lifestyle, and then there are even fewer people to talk to. It’s much easier to go through it with others than to go through it by yourself.”
The teamwork aspect is important at Carley’s Carb-less Kitchen, which has seen classes double in size in just six months of operation, leading to a move to a larger location in the Wellness Center at LAC+USC Medical Center.
“It’s not like a normal cooking class where you walk away with just a recipe,” observed Lori Eissman. “It is a teaching class where families can come together for education about MAD, eat an amazing meal and walk away with a sense of community.”
Ultimately, Carley’s Carb-less Kitchen seeks to equip families with tools to master epilepsy through food. Students quickly become the masters, taking on roles as sous-chefs, bloggers and ambassadors for the modified Atkins diet.
The Eissmans started the foundation to honor their daughter and to give back to others dealing with epilepsy. But the effort is already transforming itself.
“I’m so impressed by USC and what we’ve started and how it’s grown,” Lori Eissman said.
“I know Carley would be really proud of this.”
— Ellen Gruber
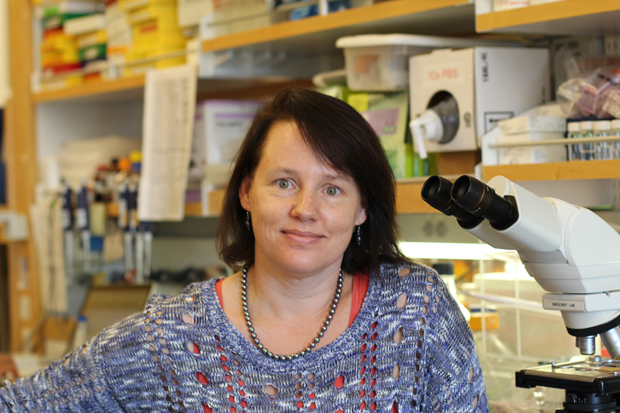
![Carley’s mother, Lori Eissman, at left in orange, helps conduct a recent cooking class that included Kesli Gazsi, Carley’s best friend, at right.]()
Carley’s mother, Lori Eissman, at left in orange, helps conduct a recent cooking class that included Kesli Gazsi, Carley’s best friend, at right.